FOI Data Reveals a Post-Code Lottery When It Comes to Counselling Through GP Practices
The #123GP campaign calls on the Minister for Health to address the huge disparities in availability of GP counselling in the department's ten-year Mental Health Strategy.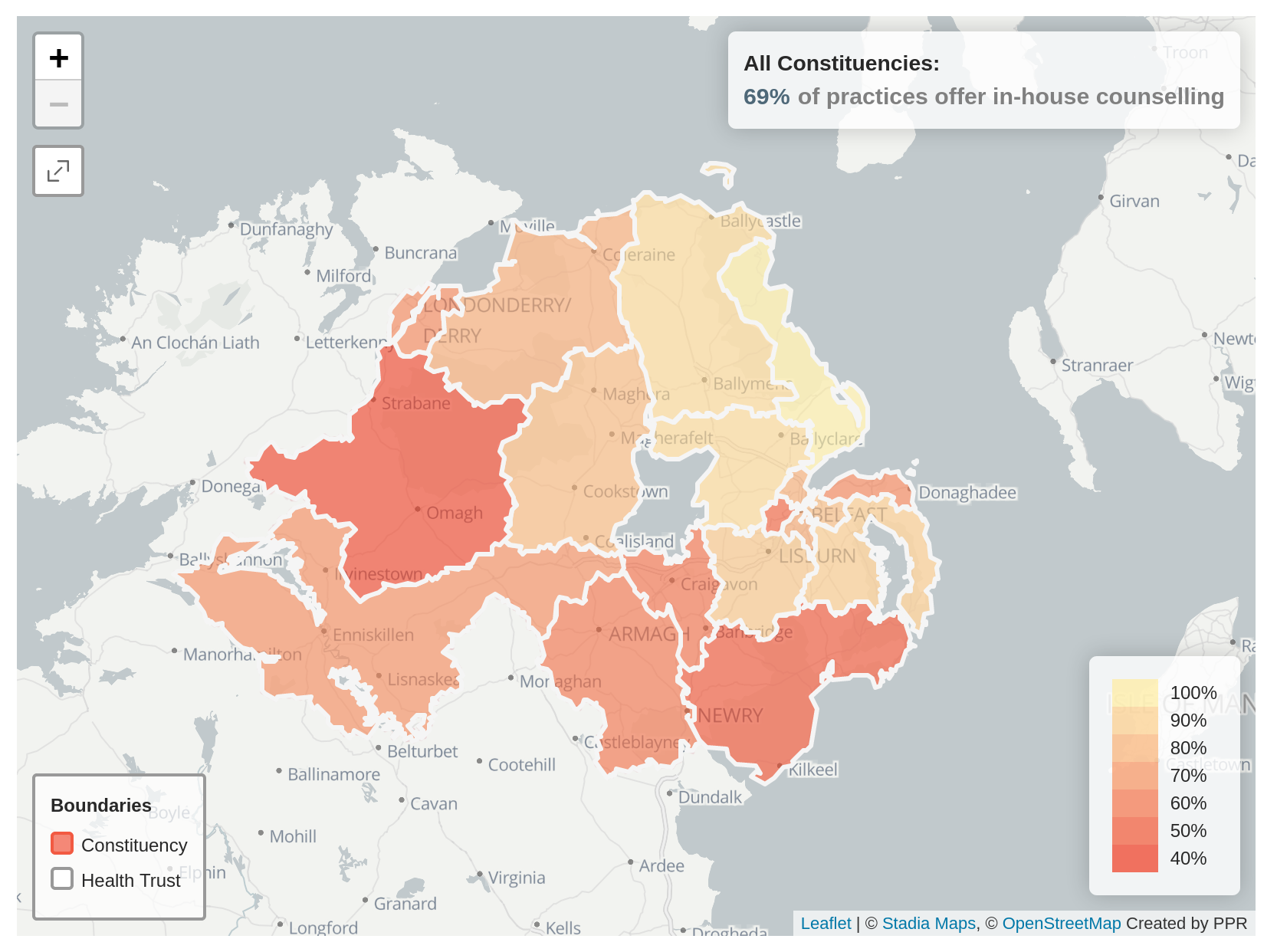
Your ability to access mental health counselling through your GP depends almost completely on where you live and there are huge disparities across the five Health Trusts and the eighteen NI Assembly constituencies.
Over 30% of GP practices are still unable to provide in-house mental health counselling, according to data obtained by PPR from the Health and Social Care Board (HSCB) as a response to a Freedom of Information request.
The data, accurate up to September 2020, and which is available for download here, reveals that a post-code lottery is in operation when it comes to GP practice-based counselling.
69% of all GP practices had an in-house counsellor, but Health Trust scores ranged from a low of 51% in the Southern Trust to a high of 89% in the Northern Trust, raising serious questions about the management of mental health services generally.
The results are even more stark when considered in terms of NI Assembly constituency areas.
PPR has been able to cross-reference the FOI data with a list of GP practices obtained from the Business Services Organisation (BSO) in order to create an interactive map to visualise the geographical deficits.
The map, available here, demonstrates that on the north coast the majority, if not all GP practices, provide in-house counselling – 100% in East Antrim and 92% in both North and South Antrim. In sharp contrast, only 40% of practices in West Tyrone, 45% in South Down and 50% in West Belfast provide in-house counselling.
Even for those GP practices that do offer in-house counselling, a range of issues have an impact on people’s ability to avail of it. These include variable waiting times, no waiting-time target or monitoring, an effective cap on the number of sessions offered, and inadequate funding.
The #123GP campaign is calling on the Minister for Health, Robin Swann, to ensure that all GP practices are equipped to provide timely access to counselling to all those who need it. To this end they are calling for the following commitments to be included in the ten-year Mental Health Strategy:
Ensure that all GP practices are adequately resourced to provide timely access to counselling for everyone who needs it.
Ensure that nobody waits longer than 28 days for a routine appointment and no longer than 2 days for an urgent one.
Provide people with options for accessing counselling – in their local GP practice or through the Talking Therapy Hubs run by the Trusts.