Post-Code Lottery for Counselling is Getting Worse, Not Better
Data uncovered by PPR via Freedom of Information has revealed a haemorrhaging of counsellors from GP practices in recent years, despite huge increases in mental health demand since Covid.
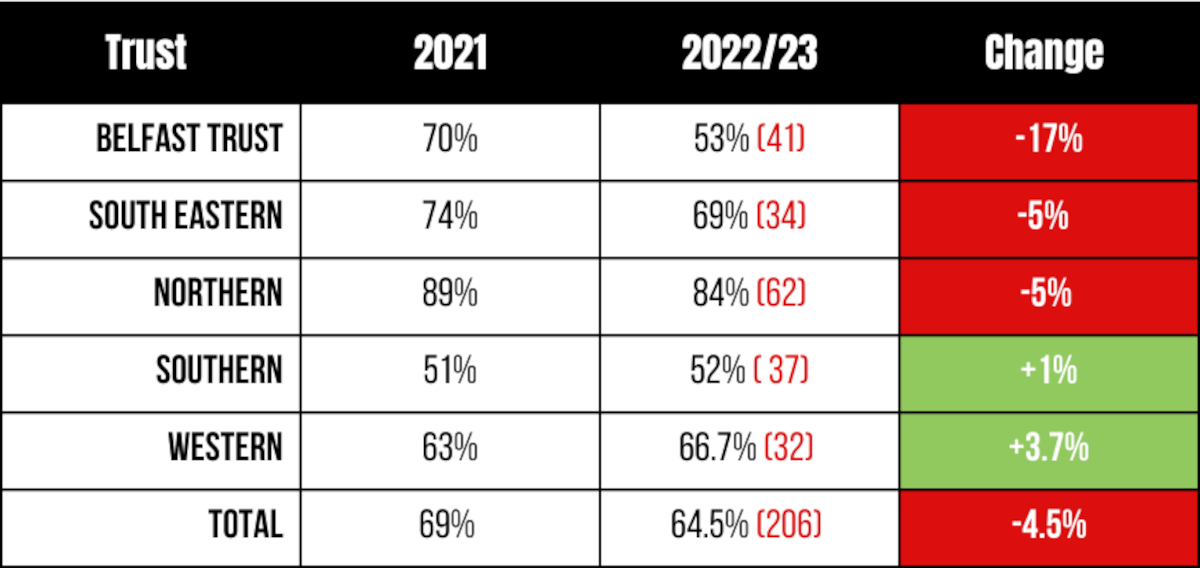
Since 2020, Belfast Trust has recorded a 17% reduction in the number of counsellors based in GP practices, while overall, there has been a reduction of 4.5% across the North. Three out of the five Trusts now have fewer counsellors working in GP practices than in 2020.
In the past year alone 13 fewer GP practices across the five Health Trusts provided in-house counselling. The majority of these practices were in the Belfast Trust area.
The post-code lottery, revealed by #123GP campaigners in 2021, continues to exist. Belfast Trust accounted for only 11.6% of all counselling sessions funded, compared to the Northern Trust which accounted for just under half (42%) of all sessions.
This reduction in vital mental health support comes at a time of spiralling mental health need.
Department of Health figures show that the number of young people waiting more than nine weeks for access to the Child and Adolescent Mental Health Service (CAMHS), more than tripled from 364 in December 2018 to 1,269 in December 2022.
There were 2,394 patients waiting more than nine weeks for access to adult mental health services in December 2022, compared to 1,579 back in December 2018.
To make matters worse, an increasing number of GP practices are closing. According to the BMA, in the past year 13 contracts have been handed back and there’s been a reduction of 30 in the past decade.
Fewer counsellors and GP practices closing all adds up to a significant worsening of access to mental health support. One of the top suggestions by people for what a New Script for Mental Health would look like, has been timely access to counselling.
No data [has been provided] on numbers of patients seen, demographic data, waiting times, number of sessions per individual or treatment outcomes.
Yet the Department of Health appears unconcerned. The only piece of performance data on in-house counselling provision required from GP practices by the Department of Health, was the number of sessions provided. No data on numbers of patients seen, demographic data, waiting times, number of sessions per individual or treatment outcomes. Unlike NHS England which collects and publishes detailed data on its Improving Access to Psychological Therapies ( IAPT).
When asked by PPR how it was addressing the geographical gaps in access to counselling, the Department of Health’s response indicated a decidedly hands-off approach, stating that‘this service is one GP practices, as independent contractors, may or may not wish to contract and provide to their patients’.
In June 2021, all political parties and a wide cross-section of civic society organisations signed the#123GP Campaign’s Consensus on Counselling. It called on the Department of Health to ensure that counselling was available to all, regardless of where they live. Almost two years later, it is clear the Department of Health has serious questions to answer.